Infertility and artificial insemination
The purpose of this leaflet is to provide information on the biological and medical nature of artificial insemination and the possible risks associated with it, the indications for artificial insemination and the legal basis for artificial insemination.
Artificial insemination of a woman is permitted using donor gametes or an embryo created from donor egg cells, regardless of her marital status, for medical indications or in the absence of a suitable male partner. The main medical indication is fertility problems, so the leaflet also covers infertility and its causes.
Definition and scope of infertility
Infertility is defined as a situation in which a woman has not become pregnant after at least a year of regular sexual intercourse (at least two to three times a week or every two to three days), even though she wishes to it. Infertility is a widespread problem, affecting approximately 15% of women.
Infertility can be primary (no previous pregnancies) or secondary (a previous clinical pregnancy is known). It is believed that approximately 30% of infertility cases are caused by female factors and 30% are due to decreased male fertility. In 30% of cases, the causes remain unclear even after thorough investigation; in some cases, both partners have decreased fertility. The most important factor in pregnancy is the woman's age, therefore a diagnosis of unexplained infertility can only be made up to 40 aged women.
Modern infertility treatment offers a range of options. The choice of treatment depends on the causes of infertility, which are determined through diagnostic testing.
Most common causes of infertility
1. Disorders of egg cell maturation and release
20-30% of the causes of female infertility are disorders of egg cell maturation and release. Egg cell maturation is regulated by hormones produced by the pituitary gland: follicle-stimulating hormone (FSH) and luteinising hormone (LH). The first stimulates the growth of a follicle containing an egg cell in the woman's ovary, while the second is necessary for the maturation of the egg cell, making it capable of fertilisation and enabling its release from the ovary (ovulation).
Follicles are fluid-filled sacs inside the ovaries where egg cells mature, and female and male hormones are produced. Disorders of egg cell maturation and release manifest as a menstrual cycle disorders (infrequent, very irregular or absent menstruation). The most common cause of menstrual cycle irregularities is the polycystic ovary syndrome, which occurs in about 10% of reproductive aged women.
Problems with egg cell maturation and release can also be caused by being underweight or overweight, thyroid dysfunction, very high levels of prolactin (a hormone produced by the pituitary gland), severe emotional stress, intense physical exertion over a long period of time and chronic illnesses. About 1% of women experience premature ovarian failure, i.e. before the age of 40. This is due to genetic predisposition or in rare cases autoimmune or inflammatory damage to the ovaries.
2. Damage to the fallopian tubes or uterine lining
Inflammation, endometriosis and surgery can damage the uterine lining and prevent embryo from implanting. Egg cells are located in the ovaries, where a woman of fertile age matures and releases (ovulates) one or two (rarely more) egg cells every month. The distal end of the fallopian tube directs the released egg cell down the fallopian tube, where it can be fertilised. The developing embryo moves along the fallopian tube and reaches the uterus on the fourth day of development, attaching to the uterine lining seven to nine days after fertilisation.
If the fallopian tubes are damaged or absent, the egg cell cannot move forward in the fallopian tube and meet the sperm, preventing fertilisation. The fallopian tubes can be damaged by inflammation, such as that caused by sexually transmitted diseases like chlamydia, gonorrhoea and mycoplasmosis. In addition, the function of the fallopian tubes can be disrupted by adhesions in the pelvic area, which may result from appendectomy, surgeries involving the reproductive organs or abdominal cavity, or endometriosis. Very rarely, there is a developmental anomaly of the reproductive organs where the fallopian tubes are not developed. A previous ectopic pregnancy is a sign of possible damage to the fallopian tubes. If it is determined that the fallopian tubes are blocked and filled with (inflammatory) fluid, such tubes must be removed before artificial insemination, otherwise pregnancy will not occur.
3. Endometriosis
Endometriosis is a chronic disease in which tissue similar to the lining of the uterus is located outside the uterus. Endometrial tissue behaves similarly to the lining of the uterine cavity; therefore, under the influence of female sex hormones, these lesions grow and partially break down, as a result they bleeding during the various phases of the menstrual cycle. Endometriosis damages the uterus and ovaries, creating an inflammatory environment in the reproductive organs and abdominal cavity and cause changes to the adhesion. The exact prevalence of endometriosis is unknown, but it is estimated to occur in 2-10% of women of fertile age and in about 50% of infertility problems women. The causes of the disease have remained unclear and its impact on the fertility depends on the severity of the disease. Endometriosis treatment is surgical or medical.
4. Causes related to the uterus
Factors that reducing the chances of conception including tumour-like changes in the uterine lining (e.g. polyps), adhesions within the uterine cavity, benign tumours in the uterine muscle layer such as fibroids (leiomyomas), congenital abnormalities in the shape of the uterus (e.g. unicornuate uterus, uterine septum), changes in the uterine muscle due to previous surgeries, narrowing of the cervix (e.g. as a result of prior surgeries).
5. Changes in sperm count and quality
The normal limit fora semen analysis is when volume of semen is at least 1.5 mL, there whereas at least 15 million sperm cells per millilitre, 40% of the sperm cells are motile, and at least 4% are of normal shape.
Causes of male infertility:
-
congenital developmental disorders (undescended testicles)
-
hormonal disorders
-
chronic genital tract inflammation
-
infectious diseases (mumps)
-
dilated testicular veins
-
chromosomal diseases and genetic characteristics
-
nervous system damage
-
previous genital trauma
-
stress and lifestyle (tobacco, drug and alcohol use; diet-related obesity, etc.)
Sexually transmitted diseases and mutations in the cystic fibrosis gene can cause damage to the sperm cells pathways.
Male infertility can also be caused by:
-
•toxic factors (heavy metals, organic compounds, alcohol, tobacco, drugs and ionising radiation)
-
medications (cytostatics, calcium channel blockers, anabolic steroids, psychotropic drugs)
A man’s fertility can be assessed using semen analysis. For the semen analysis to give accurate results, before collecting the sample the following should be avoided for two to four days:
-
ejaculation (not less than two and not more than seven days)
-
alcohol
-
sudden temperature changes (hot sauna, bath)
-
strenuous physical exertion
-
exhaustion
Artificial insemination
Artificial insemination is a procedure performed for the purpose of impregnating a woman, during which a man's sperm or an embryo, created outside the body, is transferred to the woman.
A woman can be inseminated with sperm from an anonymous donor, a non-partner donor or a partner donor. Partner donation is a gamete donation between a man and a woman who declare that they are in an intimate relationship. The man declares that the child is considered to be his descendant. Non-partner donation is a gamete donation where the identity of the donor is known to the woman, but the donor declares that the child is not considered to be his descendant. Anonymous donation is a gamete donation where the identity of the donor is not known to the woman and the donor declares that the child is not considered to be his descendant.
A sperm donor can be any adult up to 40 years of age and an egg donor can be any adult up to 35 years of age who is mentally and physically healthy and has given consent to donate their gametes for artificial insemination. With the consent of the woman wishing artificial insemination, the egg donor can be older than 35 if the donor is a relative of the woman.
The transfer of an embryo created from a foreign egg is allowed after freezing and storing it for six months, unless the woman wishes to transfer the embryo earlier after having been informed of the risks involved.
Indications and exclusions for artificial insemination
Artificial insemination for women with donor sperm is allowed regardless of marital status, for medical reasons or in the absence of a suitable male partner. Artificial insemination of a woman is permitted with an embryo, created from a foreign egg cell, only if there is a medical indication for this.
Artificial insemination is prohibited if pregnancy or childbirth threatens the life or health of the woman or the child as well as if there are other medical contraindications.
Artificial insemination is also prohibited later than one month after the death of a male partner who participated in the donation.
According to subsection 132 (1) of the Penal Code, it is prohibited and criminally punishable to transfer a foreign egg cell or an embryo created from it to a woman who intends to give up the child, developed from foreign egg cell, after birth. If a healthcare worker knows or suspects that the woman intends to give up the child developed from the embryo created from a foreign egg cell after birth, they must refuse to proceed with artificial insemination.
Voluntariness of artificial insemination
Artificial insemination is only permitted for an adult woman under the age of 51 who is legally capable and who wishes to do so. No one may force or influence a woman to undergo artificial insemination. Women may withdraw their consent in writing for artificial insemination at any time before transferring of sperm or an embryo created outside the body.
Gamete donation is also voluntary. An anonymous gamete donor is entitled to compensation. No compensation is provided to non-partner gamete donors.
Laboratory tests, the conditions and procedures for carrying out tests and the reporting of test results
Persons, whose gametes are used in the artificial insemination procedure, will undergo laboratory tests to identify markers of the following infectious agents:
-
HIV-1 and HIV-2 antibodies to detect HIV-1 and HIV-2
-
HBs antigen and HBc antibodies to detect hepatitis B
-
HCV antibodies to detect hepatitis C
-
Treponema pallidum antibodies to detect active syphilis
-
Antibody testing for HTLV I/II if the donor or their sexual partner(s) live in or come from a high prevalence area or if the donor's parents come from these areas
If the HBc antibodies are positive and the HBs antigen is negative, further testing with risk assessment will be performed to determine whether the gametes meet the requirements for clinical use.
In addition, laboratory testing for gonorrhoea and chlamydia, a peripheral blood chromosomal study, and molecular genetic testing for cystic fibrosis are performed. Genetic screening for known hereditary diseases in the family or autosomal recessive genes that cause hereditary diseases due to ethnic background is also performed to assess the risk of disease transmission. If the gamete donor lives in Estonia, a test for trichomoniasis will also be done. The woman or egg donor will also be tested for fragile X syndrome.
Blood samples for laboratory tests, except genetic tests, are collected at the time of gamete donation. For partner donation, blood samples are taken within three months prior to the first donation, and in the case of a subsequent gamete donation, blood samples are taken no later than 24 months after the previous sample.
Sperm donations, except for partner donations, are quarantined for at least 180 days. The transfer of an embryo created from a foreign egg is allowed without prior storage, written consent from the woman seeking artificial insemination is provided.
The results of the tests are reported based on an agreement between the healthcare professional and the individual(s) receiving the artificial insemination service. Your health data can also be accessed via the health portal https://www.terviseportaal.ee/.
Artificial insemination methods
All methods have one goal – to help achieve the union between the egg cell and sperm in the most natural way and to increase the chances of the egg cell getting fertilised and growing into an embryo. The ultimate goal is the development of a normal pregnancy in the uterus and a healthy baby birth. For this reason, these treatments are collectively known as artificial insemination methods. Artificial insemination methods are divided into intrauterine and extracorporeal fertilisation.
Intrauterine fertilisation
Intrauterine insemination (IUI) is performed with sperm from either an anonymous donor, a non-partner donor or a partner donor. During insemination, sperm that has been previously processed in a laboratory, is placed into the uterine cavity.
Indications for insemination include:
-
mild male factor infertility (problems with sperm count, motility or morphology; the presence of anti-sperm antibodies)
-
cervical infertility
-
unexplained infertility
-
lack of a suitable male partner
Successful insemination requires healthy fallopian tubes and a sufficient number of motile sperm cells, as well.
The likelihood of getting pregnant after insemination depends on the woman age, and the probability of getting pregnant from a single insemination procedure is about 10%.
Insemination can be performed during woman’s natural menstrual cycle or after ovarian stimulation. In the latter case, ovulation is induced by using medications. The best results are achieved when intrauterine insemination scheduled to coincide with ovulation induced by medication (ovarian stimulation). Ovarian stimulation is used to obtain up to three follicles. Tablets or injections are used for stimulation. During the stimulation, an ultrasound scan is performed to monitor follicle(s) growth. Stimulation have to performed under the supervision of a doctor to avoid possible complications (development of too many follicles, i.e. hyperstimulation). The injectable medication chorionic gonadotropin is used to schedule the egg cell release and insemination procedure. It must be self-injected under the skin at a time prescribed by the doctor.
During the presumed ovulation, a man’s sperm is prepared and transferred to the uterus using a thin catheter. The procedure is painless and does not require any anaesthesia. Insemination takes a few minutes. After that, the woman can immediately get up, go home and continue with her daily activities. For women up to the age of 40, who are insured by the Health Insurance Fund, six insemination procedures are free of charge.
If intrauterine fertilisation fails, it can be repeated a maximum of three to four times. If pregnancy is still not achieved, it is possible to switch to extracorporeal fertilisation treatment.
Extracorporeal insemination
The general term for extracorporeal fertilisation treatments is assisted reproductive technology (ART), the two most common and effective forms of which are intracytoplasmic sperm injection (ICSI) and in vitro fertilisation (IVF). After the transfer of an embryo created through extracorporeal insemination, the probability of pregnancy after one cycle of fertility treatment is around 25-30% in women under 36. This means that, in most cases, artificial insemination need to be repeated.
It has been found that the probability of live birth after six attempts is approximately 60%. The success of extracorporeal insemination depends primarily on the woman’s age and the cause of infertility.
The likelihood of becoming pregnant begins to decline for women in their early 30s and drops significantly from ages 36-37. Therefore, it is recommended to think about pregnancy, even in case of extracorporeal insemination, in the early 30s.
The only difference between the two ART treatments is the way the egg cells is fertilised. In case of IVF, the sperm penetrates the egg cell itself, whereas in case of ICSI, a selected sperm cell is directly injected into the egg cells by an embryologist. The ICSI procedure is carried out under a microscope using special equipment. It is used when the sperm is unable to penetrate through the outer layer of the egg. Once the egg is fertilised, the embryo is transferred into the uterus in the same way as with IVF.
In the incubator fertilised eggs develop for two to six days. In most cases, the embryo is transferred to the uterus on the fifth or sixth (sometimes second or third) day of development and such embryo is called a blastocyst. One, rarely two (three) embryos are transferred to the uterus at once. If more than one blastocyst is produced during extracorporeal insemination, the remaining embryos can be frozen if desired and can be used during the next seven years. Embryo freezing and cryopreservation for the first 60 days are compensated for up to 40 years old women who are insured by the Estonian Health Insurance Fund. After 60 days, the frozen embryos are stored for a fee according to the paid services price list of East Tallinn Central Hospital.
Before preparing for extracorporeal insemination, both women and men must undergo tests and examinations as prescribed by their gynaecologist (or andrologist). The whole process takes place on an outpatient basis and requires five or six appointments with the doctor.
Extracorporeal insemination is a process consisting of five stages and takes 30-50 days from the first day of preparation to the confirmation of pregnancy.
The five stages of extracorporeal insemination
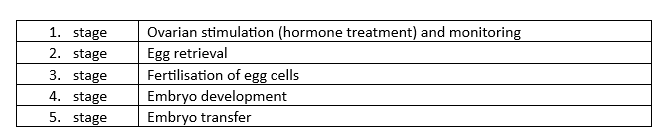
Ovarian stimulation (preparatory treatment) and monitoring
The goal of preparative treatment is to stimulate the ovaries to produce multiple follicles simultaneously (controlled ovarian hyperstimulation). To increase the chance of conception, you should have at least 15-20 mature egg cells ready for fertilisation. The woman is given injectable hormone medications (FSH, LH) to stimulate the development of the desired number of follicles in the ovaries. An ultrasound scan is performed two or three times during the cycle to monitor follicle growth; dose adjustments are made, if necessary. Certain medications are used to prevent premature ovulation. Sometimes, the effects of the medication are evaluated through blood tests to check the levels of female hormones. This phase of treatment, which stimulates the development of the ovaries, i.e. follicles and egg cells, lasts 10-14 days.
There are two main types of treatment protocols used for preparation: a short protocol using a gonadotropin-releasing hormone antagonist or a long protocol using a gonadotropin-releasing hormone agonist. The doctor will decide which protocol is more suitable for the patient. In the long treatment protocol, hormonal stimulation of the ovaries starts on day 21-22 of the menstrual cycle (a week before the expected menstruation) and the egg cell fertilisation procedure itself takes place after about a month. In the short treatment protocol, ovarian stimulation starts at the beginning of the menstrual cycle (days 2 to 5 of the cycle) and the egg cell fertilisation procedure takes place after about two weeks.
Once the largest follicles diameter is above 16-22 mm in diameter, the exact time for egg cell retrieval is determined. It is very important that 36 (32-38) hours before the egg retrieval procedure, the woman injects herself with a special medication to trigger the egg maturation process at a time scheduled by doctor.
Egg retrieval or ovarian puncture
The egg retrieval procedure is performed by using thin needle under ultrasound guidance (this is called aspiration). The procedure is performed under short anaesthesia and is therefore painless. Using the ultrasound probe as guidance, the doctor will first identify mature follicles and then pass a needle through the vagina, first into one ovary and then into the other. The needle is guided into mature follicles where it gently sucks up follicular fluid containing the eggs. All egg cells are collected from the follicular fluid and transferred to an incubator. Not every follicle contains an egg cell, and some follicles may contain egg cells that are not capable of being fertilised. The number of egg cells retrieved may be fewer than the number of follicles, the growth of which has been monitored by the doctor with ultrasound examinations. The egg cell retrieval procedure usually takes 10-30 minutes.
General anaesthesia is used to make the procedure painless. For this reason, you should stop eating and drinking opaque liquids (e.g. milk, coffee or tea with milk, fruit juice with pulp) six hours before the procedure. You should stop drinking clear liquids (clear liquids without solid particles such as water, coffee or tea without milk, fruit juice without pulp, most sugary soft drinks) two hours before the procedure. You must not chew gum or smoke for two hours before the procedure. The woman will remain under sedation only for as long as the procedure lasts. After the puncture, you will need to be observed for a few hours in the infertility treatment centre.
On average, 70% of egg cells become fertilised with the IVF/ICSl procedure.
Semen collection
The semen needed for fertilisation is collected from the man on the morning of egg retrieval. The sample is collected via masturbation in a private room at the Centre for Infertility Treatment. The semen sample may also be collected at home in a special container provided by the infertility treatment centre. In this case, the semen should be delivered to the infertility treatment centre within one hour and kept at body temperature. The man must have an identity document with him.
On the day of semen collection, the man should avoid physical exhaustion, alcohol and medication. All these factors affect sperm quality. The semen is prepared through a process called ‘semen washing’, during which the most motile sperm are separated. In the case of male infertility (problems with sperm count, motility or morphology), the sperm can be injected directly into the cytoplasm of the egg (ICSI). It is also possible to detect infections (high amounts of white blood cells in semen) and anti-sperm antibodies (the MAR-IgG test), which can affect sperm motility. The properties of semen may change over time, so a repeat analysis should be performed if necessary.
Fertilisation of egg cells
In IVF, the eggs and the sperm are put together and placed in an incubator set at body temperature. The following day, the egg cells are examined under a microscope to confirm fertilisation and to count the number of fertilised egg cells.
In ICSI, the egg cells are prepared for sperm injection by checking their maturity. In the laboratory, with great precision, a single sperm is injected directly into the cytoplasm of the egg cell, hence the name intracytoplasmic sperm injection. After about 20-24 hours, the egg cells are checked to see if it has been fertilized
Embryo development
After fertilisation, the further development of the fertilised egg cells and embryos is monitored for a maximum of seven days, usually five to six days. At the Infertility Treatment Centre of East Tallinn Central Hospital, there is a special incubator, which records embryo development in real time daily. Alternatively, once a day assessments can be made, typically 24 hours apart. This makes it possible to monitor cleavage (the division of cells) and the development of the embryos in order to select only the most viable embryos for transfer.
In most cases, the embryo is transferred on the fifth (sixth) day of its development, when the embryo 100-200 cells long. Sometimes the embryo is transferred on the second or third day after fertilisation of the egg cell, in which case the embryo is 3-5 and 8-12 cells long respectively. A very good result is considered when one third of all fertilised egg cells develop into blastocysts.
Embryo transfer
One embryo (rarely two or three) is selected for transfer to the uterus. The main criteria for embryo selection is the appearance of the cells under the microscope and do cells divide according to the expected norm rate. The embryo selected in the laboratory, which most closely matches the expected characteristics, is drawn into a fine catheter under a microscope. Using this catheter, the gynaecologist gently transfers the embryo into the uterine cavity through the vagina and cervix. The procedure is performed under ultrasound control using an abdominal sensor to ensure the correct location of the catheter. Therefore, it is necessary to come to the procedure with a moderately full bladder, which ensures the necessary visibility during ultrasound. After the removal of the catheter from the uterus, it is immediately checked under a microscope to ensure nor is the embryo stuck in the catheter.
The procedure is slightly uncomfortable but not painful, so it does not require anaesthesia. The procedure, including all the preparations, usually takes about 15 minutes. After that, you can get up immediately and resume your daily activities, including no restrictions on normal exercise or sexual intercourse.
After embryo transfer
From the day following embryo transfer, the doctor may prescribe certain medication to help maintain pregnancy. After two weeks, the woman will have a blood test to determine whether she is pregnant. An ultrasound examination can detect pregnancy on the 28th day, when the diameter of the gestational sac reaches 10 mm. You will be called for an ultrasound scan two to three weeks after a positive pregnancy test, at which time the fetal heartbeat must also be detectable.
Procedure success rates are affected by many factors, including:
-
the woman’s age
-
the cause of infertility
-
the quality of the sperm
Embryo freezing
The embryologist tries to fertilise all collected egg cells. Usually only one embryo is transferred at a time, but sometimes two, very rarely three. The remaining viable embryos can be frozen at the request of the woman and her partner – a process called cryopreservation. The embryos are stored in liquid nitrogen at -196 °C and most of them remain viable for a long time. Most embryos survive the freezing and thawing process. An advantage of cryopreservation is that these frozen embryos can be used for future transfer without having to repeat the steps of ovarian stimulation, egg retrieval and fertilisation.
According to the Artificial Insemination and Embryo Protection Act, embryos can be stored frozen for up to seven years.
Transfer of frozen embryos
Frozen embryo transfer (FET) can be used if the embryos were cryopreserved after the IVF/ICSl procedure. To prepare for the transfer of frozen embryos, different treatment regimens are used or the woman's menstrual cycle is monitored and the best time for embryo implantation is calculated. The transfer of frozen embryos is carried out in the same way as for the procedure described above. The readiness of the endometrium for the procedure is checked by two or three ultrasound examinations. Embryos are thawed on the day of the procedure.
The probability of pregnancy with frozen-thawed embryo transfer is the same or, in some cases, even better than with embryos transferred without freezing. Children born from frozen embryos are no different in terms of development from children born from unfrozen embryos or as a result of natural conception.
If after thawing the embryos it turns out that the embryos are not viable, then they will not be transferred.
Health risks associated with artificial insemination
-
Since the probability of having a child by means of assisted reproduction is 15-20% per cycle, disappointment due to the failure of the procedure is one of the most important challenges. The success of artificial insemination is most affected by the woman's age: as a woman ages, serious genetic errors arise in egg cells, which reduces fertility and also reduces the effectiveness of infertility treatment and increases the risk of spontaneous abortion.
-
Multiple pregnancy carries a higher risk of miscarriage, low birth weight and premature birth. The risk of long-term health damage to the baby due to prematurity increases.
-
The most serious complication is ovarian hyperstimulation syndrome (OHSS). In this case, the ovaries react unpredictably to the treatment, secreting biologically active substances into the bloodstream, which results in changes in blood vessel permeability and fluid moving out of the veins into body cavities, primarily into the abdominal cavity but also around the lungs and less commonly around the heart. Due to such a circulatory and blood supply disorder the risk of blood clots increases which can cause damage to the kidneys, liver and lungs. OHSS may be indicated by pain and swelling in the lower abdomen, bloating, pressure in the stomach and rectum, nausea and, in more severe cases, breathing or urination problems. If you experience any of these symptoms, contact your doctor immediately or go to the emergency department of the Women's Clinic of East Tallinn Central Hospital. Such a condition usually requires hospital treatment to prevent it from becoming life-threatening. Nowadays, the occurrence of OHSS is very, very rare because of the use of treatment regimens that minimise the risk.
-
In rare cases, the egg retrieval procedure can be complicated by bleeding (from the vagina or into the abdominal cavity). This can occur if a blood vessel is injured by a needle during ovarian puncture.
-
Very rarely, Inflammation may occur as a complication of ovarian puncture. To prevent this, an antibiotic is sometimes used before the procedure.
-
Thrombotic complications may also occur. Thrombotic complications are more likely to occur in women with OHSS.
-
In addition, artificial insemination can cause other problems. Going through fertility treatment is not always easy and there is no guarantee of success. Even if implantation is successful, there is a risk of treatment failure – miscarriage, death of the foetus (just like with natural conception).
If you experience any complications, if possible contact your doctor immediately or seek emergency care at the Women’s Clinic.
Pregnancy risk factors
Pregnancy affects a woman both physically and psychologically, presenting greater or lesser challenges at different levels. The pregnancy calendar and various risk factors can be found on the eesti.ee portal https://www.eesti.ee/et/perekond/rasedus/rasedus-naedalate-kaupa.
Medical terms are used by doctors in relation to miscarriages
-
Missed abortion – the foetus's heartbeat has stopped beating and development has stopped, but the pregnant woman may not yet have any symptoms (abdominal pain or bleeding).
-
Spontaneous miscarriage (spontaneous abortion, abortus incompletus) – the foetus has usually died and spontaneous detachment of the foetal egg from the uterus has already begun, manifested by pain in the lower abdomen and bleeding from the reproductive tract.
-
Septic miscarriage – may cause infection of the uterus, characterised by fever, chills, flu-like symptoms, abdominal pain, bleeding, foul-smelling vaginal discharge.
Risk factors for miscarriage:
-
age - the risk increases with age
-
smoking
-
alcohol consumption
-
illnesses with high fever (above 37.8 °C)
-
repeated previous miscarriages
-
trauma
-
exposure to chemicals, infections, radiation or medications, as well as mental stress
Possible causes of miscarriage
The most common cause (around 50-60% of cases) is an accidental genetic abnormality in the embryo (e.g. incorrect number of chromosomes) and an abnormality in embryo development. Miscarriage can also occur when the gestational sac develops but the foetus does not develop or dies. Chronic systemic illnesses (e.g. inadequately treated diabetes, thyroid diseases), uterine malformation, uterine fibroids may also be the cause. In most cases, it is very difficult to pinpoint a specific cause in a particular case.
Termination of pregnancy
Pregnancy termination is carried out under the Termination of Pregnancy and Sterilisation Act. A pregnancy may be terminated if it has lasted less than 12 weeks. A pregnancy that has lasted more than 12 weeks and less than 22 weeks may be terminated, if:
1) the pregnancy poses a risk to the pregnant woman's health;
2) the unborn child may have severe mental or physical health issues;
3) the pregnant woman’s illness or health problem hinders their ability to raise a child;
4) the pregnant woman is under 15 years old;
5) the pregnant woman is over 45 years old.
Gamete preservation before fertility-impairing treatment or in the presence of a fertility-impairing condition
The Health Insurance Fund reimburses gamete preservation for up to seven years for health insured women up to 35 years of age and health insured men up to 40 years of age who are about to undergo fertility-impairing treatment or have a fertility-impairing condition. After seven years, you must pay for cryopreservation yourself according to the paid services price list of the East Tallinn Central Hospital. Frozen and preserved gametes can be used for artificial insemination. Freezing gametes does not negatively affect the effectiveness of artificial insemination techniques. Gametes can be preserved for up to 12 years at the East Tallinn Central Hospital.
Counselling and consent
Before artificial insemination, the woman who wishes to undergo artificial insemination and her husband/partner and/or non-partner donor are counselled, and the parties sign the document ‘Counselling and Consent to Artificial Insemination’. Before a repeated artificial insemination procedure, all parties undergo another round of counselling and must give new written consent. Oral counselling may be waived in the case of repeated artificial insemination if the circumstances have not been changed and all parties agree with it.
A man may give written consent for his partner’s artificial insemination using anonymous or non-partner donor gametes or an embryo created from donated egg cells or through partner donation. A female spouse may give written consent to the artificial insemination of her female spouse using anonymous or non-partner donor gametes or an embryo created from a foreign egg cell. The husband's or wife's consent must be consistent with the consent of the woman. The husband or partner has the right to withdraw in writing their consent to the artificial insemination of the woman until the start of the artificial insemination procedure. In this case, the healthcare provider cannot use the donated gametes or the embryo created with them to fertilise a woman who wishes to undergo artificial insemination. Divorce automatically revokes the spouse’s consent for artificial insemination. A woman can be artificially inseminated with the sperm of her divorced husband if the husband gives a new written consent. If, after withdrawing consent, the partner donor wishes to donate gametes as a non-partner donor, both the woman and the non-partner donor must give a new written consent.
A sperm donor can withdraw his consent in writing to donate sperm at any time up to the start of the artificial insemination procedure.
An egg cell donor may withdraw her consent in writing at any time until the start of the artificial insemination procedure, or as an anonymous donor, until the start of the egg retrieval procedure.
Data collected during artificial insemination and the conditions for their processing
During artificial insemination, the following health and demographic data about the woman are collected:
1) age, place of residence, marital status
2) data on previous pregnancies, abortions, births, children and reproductive health
3) diseases and conditions suffered, including diseases and conditions suffered by close relatives
4) data on laboratory tests
5) data on lifestyle and sexual and risk behaviour
6) data on mental health
7) indication for artificial insemination
8) data on ovarian stimulation and follicular puncture
9) data on intrauterine insemination of semen
10) data on the fertilisation procedure
11) data on the transfer, freezing and thawing of embryos
12) other data necessary for the provision of healthcare services, if required
The woman's medical history will include details about previous semen testing, semen preparation and intrauterine insemination.
Non-partner gamete donors complete a health questionnaire, which collects the following health and demographic data:
1) age, place of residence, marital status
2) data on children and reproductive health
3) about diseases and conditions suffered, including diseases and conditions suffered by close relatives
4) data on laboratory tests
5) data on lifestyle and sexual and risk behaviour
6) data on mental health
Egg donors are also asked about previous pregnancies, abortions and childbirths.
The personal data of anonymous donors is not disclosed during artificial insemination. However, the woman and man who consent to artificial insemination have the right to know the following biological and social data about the anonymous donor:
-
ethnicity
-
skin colour
-
education
-
marital status
-
whether they have children
-
height
-
body type
-
hair colour
-
eye colour
The woman is provided with information about the risks associated with hereditary diseases of the gamete donor and the measures taken to prevent them.
The personal data collected during artificial insemination is processed in accordance with the Personal Data Protection Act and the Regulation (EU) 2016/679 of the European Parliament and of the Council on the protection of individuals regarding the processing of personal data and the free movement of such data, as well as repealing Directive 95/46/EC (General Data Protection Regulation).
Legal basis and consequences of artificial insemination
The legal basis for artificial insemination is set out in the Artificial Insemination and Embryo Protection Act. The parentage of a child born through artificial insemination and its legal consequences are established in the Family Law Act. The laws can be viewed on the https://www.riigiteataja.ee portal.
According to Section 82 of the Family Law Act, mutual rights and obligations of parents and children arise from the parentage established under the law. A child cannot have more than two parents.
According to subsection 84 (2) of the Family Law Act, an anonymous or non-partnered donor, whose sperm has been used for artificial insemination, shall not be recognised by the court as the father of the child.
The requirements for the procurement, handling and transplantation of gametes for artificial insemination are laid down in the Procurement, Handling and Transplantation of Cells, Tissues and Organs Act. The list of mandatory laboratory tests prescribed for donors and the conditions and procedures for conducting the tests are established by the Regulation No. 12 of the Minister of Health and Labour of 18 March 2015 ‘Criteria for the selection of cell, tissue, and organ donors, list of precluding circumstances for the donation of cells, tissues, or organs, list of mandatory laboratory studies established for a donor, and the conditions and procedure for carrying out these studies’.
Rights of a child born as a result of artificial insemination
A person who has been born as a result of artificial insemination and has reached adulthood has the right to contact the civil registry office for information about artificial insemination. If they were born as a result of fertilisation with the gametes of an anonymous donor, the following biological and social data about the anonymous donor will be disclosed to them:
-
ethnicity
-
skin colour
-
education
-
marital status
-
whether they have children
-
height
-
body type
-
hair colour
-
eye colour
Counselling options
The Women's Clinic of East Tallinn Central Hospital offers psychological and pregnancy crisis counselling services. A referral from a gynaecologist or midwife is required to register for an appointment. you can ask your hospital, midwife or gynaecologist for information about pregnancy crisis and/or psychological counselling options.
The free fertility treatment advice line of East Tallinn Central Hospital +372 5919 8395 is open every working day from 08:00 to 15:00. You can also contact the Infertility Treatment Centre by e-mail at viljatusravikeskus [at] itk.ee (viljatusravikeskus[at]itk[dot]ee).
Legal advice is provided by law firms https://advokatuur.ee/et/vajad-advokaati/eesti-advokaadiburood and other legal service providers.
If you have any questions or would like more information, please contact your doctor or the midwife at your infertility treatment centre.
ITK1154
Approved by the decision of the Medical and Nursing Care Quality Commission of Aktsiaselts Ida-Tallinna Keskhaigla on 17.12.2025 (Protocol No. 2.2-8/10-25)
 Terviseportaal
Terviseportaal