Egg donation – donation of oocytes
The purpose of this leaflet is to provide an overview of egg donation, its potential risks, and the legal framework and implications for women who wish to become egg donors.
Egg donation
Egg donation is a process in which a woman voluntarily donates her egg cells to an infertile couple or woman for artificial insemination. This can be done anonymously or the donor can donate egg cells to a specific woman.
The first recorded pregnancy using donor egg cells was reported in 1983. Egg donation is widely used in reproductive medicine and is often the only treatment option for many women to have children. Donor cells are approved for artificial insemination in women aged 18-50.
Donor egg are used for various medical indications, including:
-
ovarian insufficiency
-
ovarian dysfunction
-
premature menopause
-
chemotherapy or radiotherapy
-
genetic diseases
-
failed pregnancies through artificial insemination
Egg donation is an emotionally complex and time-consuming process. As an anonymous donor, you are entitled to receive compensation for donating egg cells, covering aspects such as your time, absence from work or travel expenses.
Who can be an egg donor?
Potential egg donors are women aged 18-35 who are mentally and physically healthy. If the donor is related to the woman seeking artificial insemination, they may be over 35 years old.
Egg donation procedure
To determine your suitability as a donor, we ask you to complete an egg donor health questionnaire and a questionnaire about your medical history and risk behaviours as well as any family history of diseases. The doctor will examine you, review your medical history and other documents proving the provision of healthcare services, and you will have the necessary tests,
including laboratory tests. Laboratory tests are necessary to prevent the transmission of infectious diseases to the woman and the transmission of genetic diseases to children. A counselling session will also be carried out, during which you will be asked to sign the document ‘Counselling and Consent for Egg Donation’. If you are an anonymous donor, an egg donation contract will be signed with you.
Laboratory tests are performed to detect markers of the following infectious agents:
-
HIV-1 and HIV-2 antibodies
-
HBs antigen and HBc antibodies to detect hepatitis B
-
HCV antibodies to detect hepatitis C
-
Treponema pallidum antibodies to detect active syphilis
-
HTLV I/II antibody test if you or your sexual partner(s) live in or come from a high-prevalence area or if your parents come from such areas
If the HBc antibodies are positive and the HBs antigen is negative, further testing with risk assessment will be performed to determine whether the oocytes meet the requirements for clinical use. In addition, laboratory testing for gonorrhoea and chlamydia, a peripheral blood chromosomal study, and molecular genetic testing for cystic fibrosis are performed. Fragile X syndrome testing is also performed as well as genetic screening for known hereditary diseases in the family or autosomal recessive genes that cause hereditary diseases due to ethnic background to assess the risk of disease transmission. If you live in Estonia, you will also be tested for trichomoniasis.
Blood samples for laboratory tests, except for genetic tests, are taken at the time of egg cell donation.
The results of the tests are reported based on an agreement between you and the healthcare professional. Your health data can also be accessed on the health portal https://www.terviseportaal.ee/.
If, as a result of the tests, you are suitable as a donor, hormonal stimulation of your ovaries will be started, the aim of which is to achieve the simultaneous maturation of several egg cells. To do this, you will need to inject yourself with hormonal medications that promote egg cell development. You will be instructed on how to inject the medications yourself. The hormones that are injected are present in the woman's body. They are given in higher doses than they are normally present in the body.
It is very important that you inject yourself on the dates and times specified in the regimen. If you inject earlier or later, your egg cells will not be usable. In this case, you will undergo an ovarian puncture, but the egg cells obtained will not be used and they will be destroyed.
You will visit your doctor two to three times during this period to determine the growth of your follicles. Once the desired diameter of the follicles has been reached, your doctor will schedule an ovarian puncture. During the ovarian puncture, follicular fluid, which usually contains egg cells, is aspirated from the follicles using a needle under ultrasound guidance.
All follicles are aspirated, but the number of egg retrieved and the quality of the egg cells vary from donor to donor. General anaesthesia is used to make the procedure painless. For this reason, you should stop eating and drinking opaque liquids (e.g. milk, coffee or tea with milk, fruit juice with pulp) six hours before the procedure. You should stop drinking clear liquids (clear liquids without solid particles such as water, coffee or tea without milk, fruit juice without pulp, most sugary soft drinks) two hours before the procedure. You must not chew gum or smoke for two hours before the procedure. The anaesthesia is short-lived and lasts exactly as long as the procedure is performed (usually 10-30 minutes).
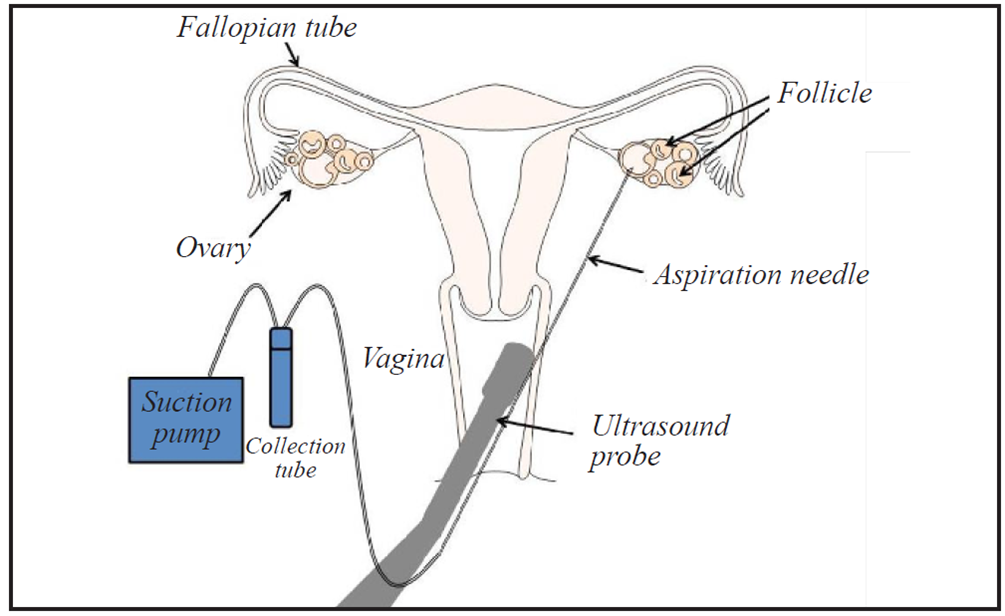
Figure 1. Ovarian puncture
Source: ASRM. Third-party Reproduction Booklet, Figure 1. Available at www.reproductivefacts.org, last accessed 08.10.2024.
After the puncture, you will stay in the hospital for a few hours for observation.
Ovarian hyperstimulation syndrome (OHSS) can occur as a side effect of hormone therapy. In this case, the ovaries react unpredictably to the treatment, secreting biologically active substances into the bloodstream, which results in changes in blood vessel permeability and fluid moving out of the veins into body cavities primarily into the abdominal cavity, but also around the lungs and less commonly around the heart. This disturbance of circulation and blood supply increases the risk of blood clots and can cause damage to the kidneys, liver and lungs. OHSS may be indicated by pain and swelling in the lower abdomen, bloating, pressure in the stomach and rectum, nausea and, in more severe cases, breathing or urination problems. If you experience any of these symptoms, contact your doctor immediately or go to the emergency department of the Women's Clinic of East Tallinn Central Hospital. Sometimes this condition requires hospital treatment. Nowadays, the occurrence of OHSS is very, very rare because of the use of treatment regimens that minimise the risk.
Very rarely, bleeding (from the vagina or into the abdominal cavity) may occur as a complication of ovarian puncture. This can occur if a blood vessel is injured during ovarian puncture. Very rarely, the procedure can lead to inflammatory complications. To prevent this, an antibiotic is sometimes used before the procedure.
Thrombotic complications have also been described in the medical literature due to the use of fairly high doses of hormone preparations. Thrombotic complications are more likely to occur in the case of OHSS. Inflammatory and thrombotic complications and bleeding are rare, but the risk exists.
If the tests reveal a confirmed risk factor or a medical contraindication to donation, you will be informed and, if necessary, your egg donation will be stopped. You have the right to withdraw your consent to donate your eggs at any time until the start of artificial insemination, or as an anonymous donor until the start of the egg donation procedure.
If you experience any complications, contact your doctor immediately or seek emergency care at the Women’s Clinic.
You are not suitable as an egg donor if you have:
-
HIV
-
acute or chronic hepatitis B, except in persons with established immunity
-
hepatitis C
-
syphilis
-
chlamydia
-
HTLV I/II
-
cystic fibrosis and other autosomal recessive diseases
-
fragile X syndrome and other X-linked recessive diseases
-
other genetic diseases
-
multifactorial developmental disorder or syndrome
-
chromosomal changes that are likely to cause unbalanced chromosome changes in the developing foetus or unborn child
As an egg donor, you are not entitled to:
-
as an anonymous donor, set preconditions for the use of your donated gametes;
-
as an anonymous or non-partner donor, demand the identification of the mother, father or child;
-
as an anonymous or non-partner donor, demand to be recognised as the mother.
According to Section 83 of the Family Law Act, the mother of a child is the woman who has given birth to the child.
If you would like more information about egg donation, please contact the Infertility Treatment Centre at the East Tallinn Central Hospital.
Health and demographic data collected about the donor
The following health and demographic data are collected about the donor:
1) age, place of residence, marital status
2) data on previous pregnancies, abortions, births, children and reproductive health
3) about diseases and conditions suffered, including diseases and conditions suffered by close relatives
4) data on laboratory tests
5) data on lifestyle and sexual and risk behaviour
6) data on mental health
7) data on ovarian stimulation and follicular puncture
8) any other data necessary for donation
If the donation is anonymous, the donor's personal data will not be disclosed. According to the Artificial Insemination and Embryo Protection Act, only the following biological and social data about the anonymous donor will be disclosed to the woman and her partner: ethnicity, skin colour, education, marital status, presence of children, height, body build, and hair and eye colour. A child born as a result of artificial insemination has the right to the same information.
Based on section 4 of the Procurement, Handling and Transplantation of Cells, Tissues and Organs Act, the donor's personal data will be processed in accordance with the Personal Data Protection Act and Regulation (EU) 2016/679 of the European Parliament and of the Council and may be disclosed only to the cell procurer, handler, transplant physician and the person who needs them to fulfil their legal obligations.
Counselling options
The Women's Clinic of East Tallinn Central Hospital offers psychological counselling services. A referral from a gynaecologist or midwife is required to register for an appointment.
The free fertility treatment advice line of East Tallinn Central Hospital +372 5919 8395 is open every working day from 08:00 to 15:00. You can also contact the Infertility Treatment Centre by e-mail at viljatusravikeskus [at] itk.ee.
Legal advice is provided by law firms https://advokatuur.ee/et/vajad-advokaati/eesti-advokaadiburood and other legal service providers.
If you have any questions or would like more information, please contact your doctor or the midwife at your infertility treatment centre.
Thank you for choosing to become an egg donor!
ITK1295
Approved by the decision of the Medical and Nursing Care Quality Commission of Aktsiaselts Ida-Tallinna Keskhaigla on 17.12.2025 (Protocol No. 2.2-8/10-25)
 Terviseportaal
Terviseportaal