Treatment of surgery-related oedema of the extremities
The purpose of this leaflet is to explain to the patient the reasons behind post-surgery oedema of the extremities and to provide recommendations for treatment and self-help.
Post-operative oedema
Post-operative oedema (swelling) is the body’s normal physiological response to surgery, an inflammatory process associated with the build-up of excess fluid (blood plasma, lymphatic fluid, blood, tissue fluid, and inflammatory fluid) in the tissues. Swelling usually occurs within the first 24 to 48 hours after surgery and reaches its maximum within 72 hours, in rare cases within 120 hours. Postoperative oedema usually resolves within the first 2 weeks, but in some cases may persist for 3–6 months. In patients with chronic disease (e.g. diabetes, venous failure, obesity), swelling may become chronic.
In most cases, swelling occurs only in the surgical area, but sometimes it can spread throughout the limb, moving upward along the extremity, or expanding along the lymphatic pathway. Post-operative swelling is often accompanied by symptoms such as pain, tension, reduced muscle activity and range of movement of the joints, discolouration of the skin, haematomas, sensitivity disorders, and even blisters. Swelling should be prevented. It is also very important to treat the swelling immediately to prevent it from worsening and to avoid post-operative complications (e.g. blood clots). As swelling gets worse, the healing process slows down, which in turn can lead to chronic restrictions on joint mobility and reduced muscle strength in the future.
Treatment of post-operative oedema
Treatment of post-operative oedema is conservative. Treatment of oedema begins immediately in the postoperative department and should be continued at home, if necessary. Treatment recommendations are given by a doctor, nurse, physiotherapist or occupational therapist. Various methods described below are used for the treatment of oedema.
-
Positioning therapy
Positioning therapy is very important. The movement of human body fluids is affected by gravity, and keeping the limbs in the right position promotes the drainage of excess fluid. The swollen limb is lifted at least 3–4 times a day above the cardiac and trunk levels for 20–30 minutes.
In the case of the swelling of the lower extremities, lie on your back or sit down and place cushions or other elevations under your leg (Figure 1). In the case of the swelling of the upper extremities, you may also lie on your back or side, or assume a seated position and use pillows to raise your extremity (Figures 2 and 3). After receiving instructions from a healthcare professional, you can perform positioning therapy on your own. If necessary, you will be assisted by a nurse or caregiver. When at home, ask for help from loved ones.
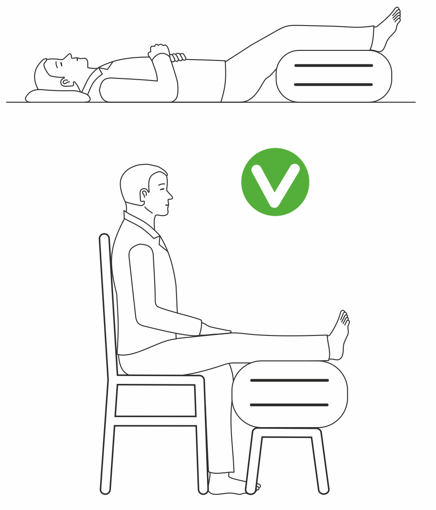
Figure 1: Position recommendations in case of swelling of the lower extremities
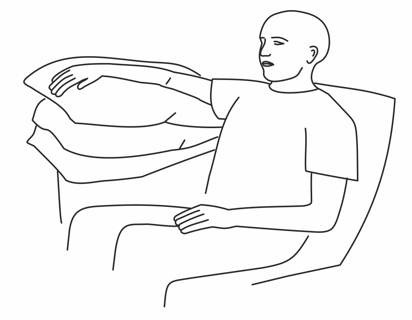
Figure 2: Position recommendation in case of swelling of the upper extremities when seated
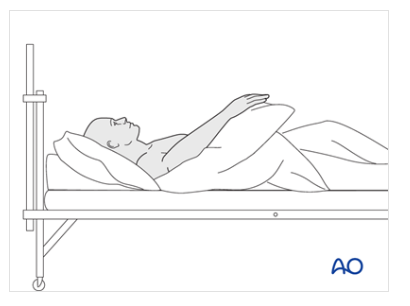
Figure 3: Position recommendation in case of swelling of the upper extremities while lying down Source: AO Surgery Reference, https://surgeryreference.aofoundation.org. Copyright: AO Foundation, Switzerland
-
Cold treatment
The most popular method of treatment of swelling is cold therapy. This treatment includes cold compresses, bags and wraps, which should be used at least 3–4 times a day for 15–20 minutes until the swelling improves. A cold gel pack is not placed directly on the skin. An intermediate layer, such as a terry towel, should be placed between the skin and the pack to prevent frostbite. You can place cold gel packs on the swollen area yourself after receiving instruction.
In addition, a cold compression device is used, which simultaneously performs a massage and cold treatment that promotes fluid drainage with alternating pressure on the extremity. It is recommended that this device be used once a day for 30 minutes. Such devices are available in different departments in the hospital (orthopaedics and rehabilitation). The cold compression procedure is subject to a fee and is prescribed by a doctor on the basis of a referral.
-
Compression therapy
Compression clothing, bandages, stockings, and compression devices help prevent and reduce post-operative swelling. Compression of the limb reduces excess soft tissue volume so that the swelling fluid cannot easily accumulate in the tissues. Stockings and bandages with the right pressure (stronger in the foot, slightly weaker in the lower leg) prevent swelling and facilitate the movement of blood and tissue fluid away from the swollen area, resulting in a reduction in swelling. Patients are often advised to purchase compression stockings from a technical aid supplier or lymphatic oedema treatment centre. Sometimes, your doctor will refer you to a lymph therapist for lymph therapy, before prescribing stockings. If you are already undergoing lymphatic therapy and are wearing compression garments, your doctor will issue a prescription to purchase compression products on the basis of a medical device card. To treat oedema and prevent complications, you can also contact lymphatic specialists, such as lymphatic therapists, who provide paid services.
-
Lymphatic therapy
Lymphatic therapy is a method aimed at freeing the lymphatic vessels, improving lymph circulation and drainage, and reducing swelling through compression binding. The lymphatic therapist performs lymphatic drainage with massage and compression therapy using bindings and special devices. Lymphatic therapy helps to speed up recovery and prevent complications associated with swelling and dysfunction of the lymphatic system. Lymphatic drainage massage is always performed in the direction of natural lymphatic flow to promote lymphatic fluid drainage and prevent stagnation (Figure 4). In case of more severe oedema, lymphatic therapy should be performed under the supervision of a doctor, taking into account possible contraindications and the risk of complications (for example, in case of a risk of infection or thrombus, or in case of severe heart failure).
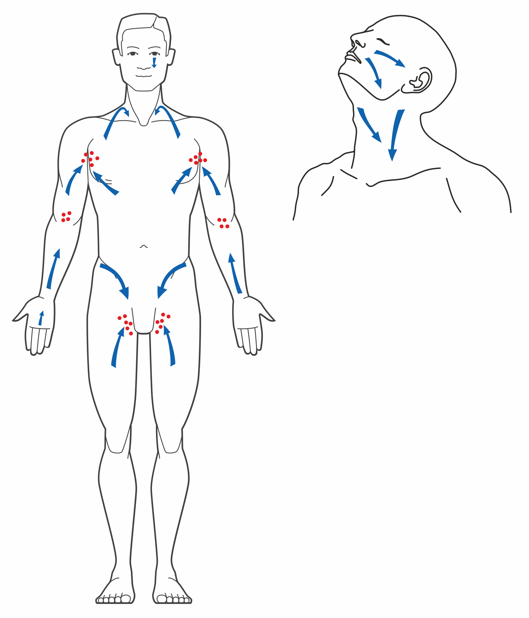
Figure 4: Lymph drainage massage directions in case of swelling
-
Physiotherapeutic exercises
Inactivity after surgery increases the likelihood of developing swelling, so it is very important to start exercising early. Depending on the type of surgery, initial exercise restrictions or a pre-existing condition may limit mobility, which in turn makes it difficult to maintain and increase the level of post-operative physical activity. However, even if active movement is impossible, there are several methods for reducing and treating the risk of swelling, including simple exercises. For example, exercises that improve lymphatic drainage and blood circulation can be performed to treat swelling and lymphatic oedema. If you are unsure about how to do the right exercises and move during recovery, your attending physician or physiotherapist will be able to offer useful advice.
-
Kinesio taping
Kinesio taping can be used to improve blood and lymph circulation, as well as to relieve swelling and pain after surgery. It helps to support damaged tissues, relaxes muscles, and speed up the recovery process. The anti-swelling Kinesio taping technique is mainly used to reduce post-operative swelling in the lower extremities. Kinesio taping is performed by a physiotherapist or lymphatic therapist, who will often teach the patient how to apply the tape themselves at home. Figure 5 shows an example of Kinesio taping for lower limb swelling.
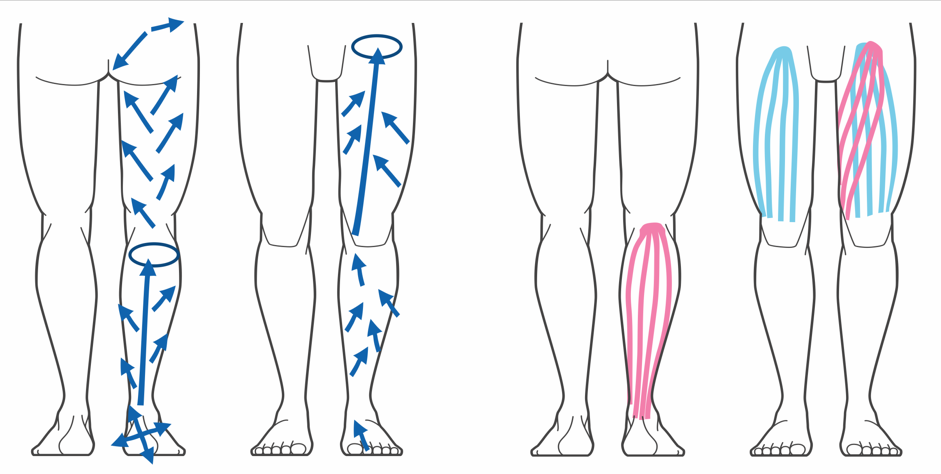
Figure 5: Kinesio taping of lower limbs in case of swelling
-
Device treatment: Electrical and Magnetic Therapy
Electrical and magnetic therapy is used, if necessary, as a supportive method for the treatment of postoperative oedema. During electrical therapy, electrical impulses stimulate tissue to improve microcirculation and lymphatic drainage, thereby reducing swelling. Magnetic therapy improves blood circulation and relieves pain and inflammation.
These methods are used in rehabilitation and can also be used after surgery to speed up the patient’s recovery. Despite their high efficiency, contraindications should also be taken into account when using electrical therapy. Pulse and magnetic therapy cannot be used if you have a pacemaker or other implanted electronic devices (e.g. insulin pump, etc.), as it may interfere with the functioning of the implanted device(s). Also, the presence of joint prostheses or metals in the body, acute inflammation, infection, tumours, blood diseases or individual intolerance to the methods of treatment may be contraindications to the use of therapeutic devices. Before using electrical and magnetic therapy methods, it is important to consult a doctor, who will assess their feasibility and the safety of treatment on a case-by-case basis.
In the case of oedema, combining the above methods of treatment is the most effective way to prevent postoperative complications and accelerate recovery. For example, cold therapy, combined with the wearing of compression garments, effectively helps to reduce swelling and inflammation, while at the same time providing the muscles and vascular system with necessary relief. It is also important to combine exercise with elevating the limb, thus promoting blood circulation and improving lymph flow.
In the case of a postoperative oedema, it is important to avoid prolonged standing or sitting, as these activities can slow blood and lymph circulation and even lead to an increase in oedema. When seated with your legs below your heart, blood and lymph circulation in the groin is impeded and drainage back into the larger circulation is slowed, causing fluid to accumulate.
Also, excessive physical exertion or complete inactivity, such as bed rest, can worsen recovery and lead to the persistence of swelling. Therefore, performing anti-swelling exercises while on bed rest is also of paramount importance.
Obesity, the use of heat therapy, as well as advanced age are factors that can slow down the treatment of swelling and the recovery process. Therefore, it is important to follow a healthy lifestyle, be active, exercise regularly with moderate loads, and consult with specialists to choose appropriate treatment methods.
ITK1290
Approved by the decision of the Medical and Nursing Care Quality Commission of Aktsiaselts Ida-Tallinna Keskhaigla on 12.November 2025 (Protocol No. 2.2-8/8-25)
 Terviseportaal
Terviseportaal