Congenital blockage of the tear ducts in infants
The purpose of this information material is to explain to the parent the nature and treatment of congenital blockage of the tear ducts in infants.
It is not uncommon for one or both of a baby’s eyes to become watery and crusty during the first or second month of life. In most cases, this is caused by congenital obstruction of the tear ducts. Symptoms do not manifest themselves immediately at birth, due to the fact that the lacrimal gland is not fully developed. However, if tear production increases, symptoms will occur: the eye becomes watery and may begin to crust. At the same time, the eyeball itself is white and there is no redness in the conjunctiva (the conjunctiva is a thin transparent membrane that covers the front of the eye and lines the inside of the eyelid). When pressure is applied to the tear duct in the area of the nasal bridge a discharge may come out of the tear ducts (see Picture 1).
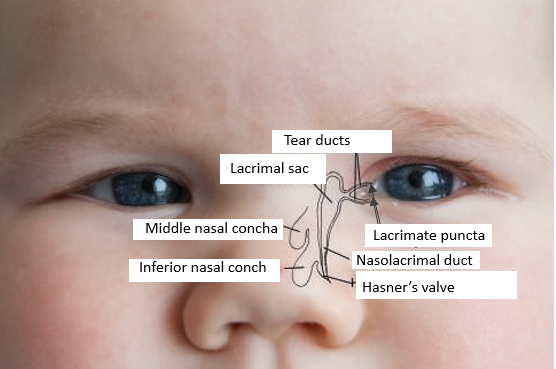
Picture 1: Anatomy of the tear ducts
Reason for closure
At the end of the nasolacrimal duct there is a small membranous fold, or Hasner’s valve, which may be closed at birth in as many as half of newborns, but most of the time it opens spontaneously within a period of about 3 weeks. In the case of approximately 5–10% of infants, it does not open at the right time and symptoms of tear duct blockage develop: wateriness and crustiness of the eye.
Diagnosis and treatment
In most cases, a conversation between the doctor and the child’s parent, along with external observation, is enough to provide a diagnosis.
The most important treatment is massage of the tear duct. First, it drains the tear duct and reduces the likelihood of bacteria spreading. Secondly, massaging creates hydrostatic pressure on the blockage, which can sometimes open the blockage and solve the problem. If there is a large amount of puss, it is recommended, for example, to use chloramphenicol drops prescribed by a family physician or ophthalmologist, or OCUflash® drops available over the counter.
How to perform the massage?
To perform the massage, place your finger on the bridge of the nose (see Picture 2), press firmly against it and push your finger downwards, following the direction of tear drainage. There are different techniques for performing a massage, one of which involves 10 presses 4 times a day.
The massage is performed until the symptoms disappear or until the decision is made to perform tear duct probing. The duration of the symptoms varies, and the decision to perform probing will be made by your doctor after a consultation with you.

Picture 2: Tear duct massage
Sometimes probing is necessary.
If the problem persists despite the massage, probing of the tear ducts is necessary. A probe is inserted into the tear ducts through the lacrimal punctum, through which the tear ducts are flushed with a physiological solution; this opens Hasner’s valve. This is done in most cases in infants between 6 and 12 months of age and, depending on the hospital, either under local anaesthesia (anaesthetizing the surface of the eye, dripping numbing drops) or general anaesthesia (the child is put to sleep for a short period of time with the help of medications). At East Tallinn Central Hospital, local anaesthesia is mostly used in children under 1 year of age, as smaller children can be held safely, thus reducing the need for general anaesthesia. For children over 1 year of age, probing is usually performed under general anaesthesia.
After probing, there may be slight bleeding from the nose or tear duct, but this does not require any treatment. After the probing, it may be necessary to use anti-inflammatory eye drops, which will be decided by the doctor who performed the procedure.
A small number of newborns may have anatomical features that mean probing alone may not be sufficient.
If the child has undergone probing before the age of one, but the symptoms persist, then probing is performed again under general anaesthesia. If this also does not help, surgery called bicanalicular silicone intubation is necessary. During this procedure, a silicone tube is inserted into the tear ducts to ensure that the tear ducts are open under scar tissue conditions. The operation is performed under general anaesthesia, and the child usually is allowed to go home a few hours after the anaesthesia wears off.
It is important that the child does not rub their eyes too hard after the surgery, as the tube may stretch the tear ducts if pulled too hard. A small amount of bloody tears and bloody discharge up to 2 weeks after the procedure does not require separate treatment. The silicone tube is left in the tear pathways for 1–3 months and is removed in most cases under general anaesthesia.
ITK1292
Approved by the decision of the Medical and Nursing Care Quality Commission of Aktsiaselts Ida-Tallinna Keskhaigla on 12.November 2025 (Protocol No. 2.2-8/8-25)
 Terviseportaal
Terviseportaal