Implantation of a cardiac pacemaker
The purpose of this leaflet is to provide the patient with information about the implantation a cardiac pacemaker.
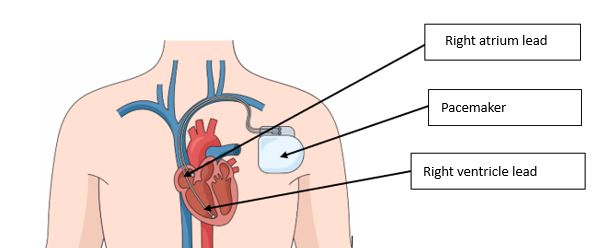
Figure 1: Location of the cardiac pacemaker
A cardiac pacemaker or simply pacemaker is a device that uses short electrical pulses to prevent a heart rate that is too slow. The device consists of a pulse generator, or battery, and fine electrodes, or wires, that conduct pulses into the heart muscle. A pacemaker is implanted if an excessively slow heart rate causes symptoms such as weakness or loss of consciousness, or if there are arrhythmias that cannot be effectively treated without the support of a pacemaker.
Having a pacemaker does not restrict your daily activities or mobility; its purpose is to improve quality of life and the performance of the heart.
Before the procedure
You will usually be asked to come to the hospital the day before the procedure. You can eat and drink as normal in the morning and take your usual medications, with the exception of antithrombotic medications or blood thinners. Ask your doctor at the time of referral for more information on the use of blood thinners.
You will be given antibiotics before and after the implantation to prevent possible bacterial inflammation of the wound area.
Attention!
If you are allergic to antibiotics, anaesthetics, or contrast agents, please be sure to inform your doctor!
Before the procedure, please read the information about the pacemaker that will be inserted in the hospital. If you have any questions, you can ask your doctor.
Procedure
A pacemaker is implanted in the operating room. In general, the procedure is carried out with local anaesthesia. A cut of 4–5 cm in length is made below the collarbone, usually on the left side of the body. Electrodes are then introduced into the heart cavity through a vein in the same area. The cardiac stimulator is then placed under the skin on the left breast muscle, after which the wound is closed with stitches.
After the procedure
-
A weighted bag will be placed on the wound area for about two (2) hours to prevent bleeding. You can move around once the weight has been removed.
-
You can eat and drink immediately after the procedure.
-
In general, an X-ray of the chest is taken to make sure that the procedure has been uneventful.
-
You will usually be discharged from the hospital the day after the procedure.
-
On the day you go home, you will be provided with a pacemaker implantation document indicating the date and time of your first follow-up appointment. You will also be given a pacemaker passport, which you are advised to carry with you at all times.
After discharge from hospital
-
The wound will be covered with a waterproof patch that you can remove after 10 days.
You can wash yourself in the shower, but you should avoid baths and saunas for two (2) weeks after the procedure.
-
In case of wound pain, you can take painkillers.
-
Wound suture threads are removed 10 days after the procedure; this is done by
a cardiology nurse or family physician/family nurse in their office. If an absorbable suture has been used, the removal of threads is not necessary.
-
For the first two (2) weeks, avoid stretching the shoulder area and lifting your hand above your head.
-
If necessary, read the pacemaker information again.
-
After the wound has healed, you can return to your normal routine.
-
Travel and air travel are not limited. When passing through security, you may be asked to present a pacemaker passport or card.
-
The first follow-up appointment with the doctor to check the operation of the pacemaker is 1–2 months after implantation.
Emergency medical advice should be sought if you experience any of the following:
-
Decrease in heart rate below the programmed heart rate (e.g. less than 55 beats per minute), this parameter will be explained to you by a cardiologist.
-
Reoccurrence of pre- implantation symptoms (e.g. dizziness or fainting).
-
Symptoms of inflammation, such as swelling, redness, pain in the wound area and purulent discharge, or increased body temperature not associated with any other disease.
Possible complications
Although significant complications following the implantation of a pacemaker are rare (occurring in less than 5% of procedures), hospitalisation may be necessary if they occur.
-
The risk of wound bleeding or severe bruising is higher when blood thinners are used.
-
If a pneumothorax or collapsed lung has occurred during the procedure, it will be necessary to install a temporary drainage system in the pulmonary cavity.
-
Disconnection of the pacemaker from the place of attachment of the electrode requires that the procedure to secure the electrode be repeated.
-
Inflammation in the wound or on the surface of the electrode often requires long-term treatment with antibiotics and the removal of the pacemaker from the site of inflammation.
If you have any questions or need more information, please contact your doctor or ask for advice on the helpline for patients with pacemakers 620 7426 on weekdays from 8–16.
ITK1281
Approved by the decision of the Medical and Nursing Care Quality Commission of Aktsiaselts Ida-Tallinna Keskhaigla on 27. August 2025 (Protocol No. 2.2-8/3-25)
 Terviseportaal
Terviseportaal